It may surprise you, but around 1 in 250 people have familial hypercholesterolemia (FH). This is a genetic condition that makes it hard to manage cholesterol. Because nearly 1 in 3 adults deals with high cholesterol, it’s critical to know if it’s genetic. Understanding this can help protect the heart health of many families.
Genetics play a big role in our cholesterol levels. Those with inherited high cholesterol are at a greater risk for heart problems. They need quick action to avoid serious health issues. Hopkins Medicine shares important insights on how genetics affect cholesterol.
We’re taking a closer look at how genetics might set our cholesterol levels. This will help us understand if high cholesterol can really be passed down in families.
Key Takeaways
- Familial hypercholesterolemia affects about 1 in 250 people.
- Untreated FH can increase the risk of coronary heart disease by up to 13 times.
- Early diagnosis and treatment of FH help individuals live as long as those without the condition.
- Genetic predispositions can influence unhealthy behaviors, impacting cholesterol levels negatively.
- Lifestyle changes combined with medication can effectively manage hereditary high cholesterol.
Understanding Cholesterol and Its Importance
Cholesterol is a waxy substance that’s vital for making cells and hormones. It travels in our blood encased in lipoproteins. Low-density lipoprotein (LDL) is known as “bad” cholesterol, while high-density lipoprotein (HDL) is called “good.”
Having the right balance between LDL and HDL is key because high LDL can lead to heart disease and strokes.
Eating foods rich in saturated fats like red meats can increase LDL. Not exercising enough lowers HDL, which is bad because HDL helps eliminate harmful cholesterol. Smoking also lowers HDL and raises LDL, harming your health.
Stress can make the body produce more cholesterol. Drinking too much alcohol raises your cholesterol, too. Also, some people inherit high cholesterol risks from their parents through a condition called familial hypercholesterolemia (FH).
As we age, cholesterol levels usually go up. Men under 39 and post-menopausal women have higher risks of bad cholesterol. Family history and diseases like diabetes also affect your cholesterol.
Being overweight links to higher cholesterol levels. It’s crucial to live healthily to manage cholesterol. Getting regular checks can help find any problems early, preventing serious issues later on.
What are Cholesterol Genetics?
Cholesterol genetics are key in how our bodies handle cholesterol. They greatly affect our cholesterol production, especially LDL, the “bad” cholesterol. A common issue related to these genetics is Familial Hypercholesterolemia (FH). It impacts around 1 in 200 adults. In the U.S., about 1.3 million people, including kids, have FH. Shockingly, only 10% know they have it.
FH is passed down in a certain way, due to changes in specific genes like LDLR, APOB, or PCSK9. If you get the FH gene from one parent, you may have LDL levels over 190 mg/dL. Getting the gene from both parents can push LDL levels above 400 mg/dL. Studies show 60-80% of FH cases involve a mutation in one of these genes.
Knowing about cholesterol genetics is not just for diagnosis. It helps in screening relatives early, which can save lives. If found early, people with FH can greatly lower their heart disease risk. The key is in lifestyle changes and taking the right meds. This shows why it’s vital to recognize how genetics play a role in cholesterol.
Is High Cholesterol Genetic? Exploring the Connection
Research shows that our genes can greatly affect our cholesterol levels. Conditions like familial hypercholesterolemia (FH) are passed down through families. It’s important to understand how these issues come about. This helps us grasp their widespread nature and the need to take action.
The Role of Genetics in Cholesterol Levels
Many times, high cholesterol is in our family’s genes. FH is a common genetic condition, found in 1 out of every 300 people worldwide. Around 34 million people suffer from it. Shockingly, 90% of them don’t know they have it. This puts them at a higher risk for heart problems. Having relatives with high cholesterol also ups your own risk, showing how genes are key in this issue. For more details, click here.
Inherited Cholesterol Disorders and Their Prevalence
Familial hypercholesterolemia is a big public health issue. Yet, many people don’t know about it. Some countries, like Slovenia, have made great strides. They’ve bumped up diagnosis rates from 1% to about 20% in 15 years. Turkey is also getting on board, creating registries to better understand and tackle FH.
Spotting and managing these genetic cholesterol issues early is key. Lifestyle changes help, but they might not be enough for those with FH. Screening and genetic tests are good moves if high cholesterol runs in your family. By taking these steps, people can better handle their conditions. This lowers their chances of heart disease.
Familial Hypercholesterolemia (FH): A Closer Look
Familial hypercholesterolemia (FH) is a major genetic disorder. It causes high cholesterol levels because the body can’t remove LDL cholesterol well. Knowing the key factors and those at risk can lead to early spotting and active care.
What is Familial Hypercholesterolemia?
Familial hypercholesterolemia (FH) is mainly a genetic issue that leads to very high cholesterol. This can often result in heart problems. Worldwide, between 14 to 34 million people have FH. Most cases, about 85% to 90%, are due to changes in the LDL receptor gene.
Other changes, like in the ApoB gene and sometimes PCSK9 gene, make a smaller part of FH cases. This genetic risk makes heart health very important to watch.
Who is Most at Risk for FH?
Certain groups have more cases of FH than others. These groups include Christian Lebanese, French Canadians, Dutch Afrikaners, Ashkenazi Jews, and Asian Indians. They see rates as high as 1 in 50 to 1 in 100. The less severe form happens in about 1 in 300 to 1 in 500 people. The very severe form is super rare, at 1 in 1,000,000.
Things like lifestyle can add to the risks of FH, making it crucial to know if you’re at risk.
| Population | Estimation of FH Prevalence |
|---|---|
| Christian Lebanese | 1 in 50 to 1 in 100 |
| French Canadians | 1 in 50 to 1 in 100 |
| Dutch Afrikaners | 1 in 50 to 1 in 100 |
| Ashkenazi Jews | 1 in 50 to 1 in 100 |
| Asian Indians | 1 in 50 to 1 in 100 |
| General Population (HeFH) | 1 in 311 |
Knowing about familial hypercholesterolemia and its risks is vital, as many people don’t know they have it. Finding and treating it early can cut down on severe heart diseases a lot.
Identifying Early Signs of High Cholesterol
Finding early signs of high cholesterol can be hard because most people don’t show clear cholesterol symptoms. Knowing what to look for is key to taking care of your health early. Look for xanthomas, which are fatty deposits, as a hint of too much cholesterol. Spotting these early can be very important for stopping bigger problems.
Physical Symptoms to Watch For
Many with high cholesterol won’t feel different, but there are signs to look for, including:
- Xanthomas: Yellowish, fatty lumps that might show up on your skin.
- Xanthelasma: A kind of xanthoma that appears specifically on the eyelids.
- Corneal arcus: A white or gray circle around the eye’s cornea.
Spotting these signs early can suggest it’s time for a healthier lifestyle or seeing a doctor.
Importance of Family History
It’s crucial to look into your family’s health history. Some groups have a high chance of having conditions like familial hypercholesterolemia (FH). Sadly, over 90% of people with FH remain undiagnosed. Knowing your genetics is important since it can raise your risk of high cholesterol and heart issues. Talking to doctors and using resources like family history information can be very helpful.
Actively checking and talking about cholesterol in your family can lead to better health. By knowing your family’s health history, you can find and address high cholesterol sooner. This highlights why knowing and educating about cholesterol is so significant.
Genetic Factors Affecting Cholesterol Levels
Genes play a major role in someone’s cholesterol levels. Knowing about genetic factors helps catch and manage high cholesterol early. This is vital for those who have a family history of this condition.
Cholesterol Gene Mutations
Changes in cholesterol genes greatly influence how the body handles cholesterol. Familial hypercholesterolemia (FH) is a key example, mainly due to LDL receptor (LDLR) gene mutations. People with these changes often have high LDL cholesterol. This increases their heart disease risk. Genetic testing can spot these changes, guiding how to control cholesterol. About 60-80% of FH cases are because of changes in LDLR, APOB, or PCSK9 genes.
How Genetic Influences Impact Health
But it’s not just FH. Other genetic factors can push cholesterol up. This mix of genetics and lifestyle makes it harder to keep cholesterol in check. This can lead to more atherosclerosis. Watching cholesterol levels closely, especially if they are above 170 mg/dL, is key. It helps find who might need genetic testing and treatment. Regular blood tests show if treatments are working or not for those at genetic risk.

| Population | Prevalence of FH |
|---|---|
| Black people | 1 in 211 |
| White people | 1 in 249 |
| Mexican Americans | 1 in 414 |
| Other ethnicities | 1 in 343 |
By understanding cholesterol gene mutations and their effects, doctors can better help their patients. This personalized approach improves health outcomes.
Testing and Diagnosis of High Cholesterol
Understanding how to test for high cholesterol is key in catching and managing it early. The first step is usually a fasting blood test that checks your blood for lipoproteins. If you might have familial hypercholesterolemia (FH) because it runs in your family, you might need more tests. Genetic testing can help figure out if you have FH.
How to Get Tested for High Cholesterol
To get tested for high cholesterol, go see your healthcare provider. They’ll likely suggest a fasting lipid panel. This test looks at your total cholesterol, LDL (bad) cholesterol, HDL (good) cholesterol, and triglycerides. You’ll need to fast for 9 to 12 hours before the test. This helps decide if more tests are needed, for example, if you have symptoms or a family history of FH.
Importance of Genetic Testing
Genetic testing is very useful for people who might have FH. It can find the genetic cause in about 60%–80% of those tested. Knowing if you have a genetic change helps figure out the best treatment. It also lets your family know if they should get checked.
But sometimes, genetic testing doesn’t give clear answers. You might get results that are hard to understand, like a variant of uncertain significance (VUS). In these cases, talking to a genetic counselor can help make sense of the results.
| Genetic Testing Outcomes | Percentage of Cases |
|---|---|
| Genetic Change Causative of FH Found | 60%–80% |
| No Genetic Change Detected | 20%–40% |
| Variant of Uncertain Significance | Varies |
| Familial Hypercholesterolemia Incidence | 1 in 250 |
| Homozygous Familial Hypercholesterolemia | 1 in 1,000,000 |
For those at risk, getting tested for high cholesterol and considering genetic tests is critical. It makes sure you get the right care and treatment plan.
Management and Treatment Options for High Cholesterol
High cholesterol treatment includes lifestyle dietary modifications, medication, and monitoring. People should embrace heart-healthy habits and use medicines as needed. This helps keep cholesterol levels in check.
Lifestyle Changes and Diet
Making lifestyle changes is key to controlling high cholesterol. These changes can include:
- Adopting a low-saturated-fat diet.
- Increasing intake of fiber-rich foods such as fruits, vegetables, and whole grains.
- Incorporating regular physical activity, aiming for at least 150 minutes of moderate exercise weekly.
- Maintaining a healthy weight, as losing even a small percentage of body weight can positively influence cholesterol levels.
- Limiting alcohol consumption and entirely avoiding smoking.
These lifestyle dietary modifications can reduce heart disease risk. They may also lessen the need for heavy cholesterol treatment.
Medications for Managing High Cholesterol
People with conditions like familial hypercholesterolemia (FH) often need medication. Statins are common for lowering LDL cholesterol. Options include:
- Atorvastatin (Lipitor)
- Simvastatin (Zocor)
- Bempedoic acid, which has a lower risk of muscle pain than statins.
Some may also need medications like ezetimibe or PCSK9 inhibitors. These include alirocumab (Praluent) and evolocumab (Repatha). For serious cases, treatments like lipoprotein apheresis or liver transplants might be critical.
For more info on cholesterol treatment options, talk to healthcare experts.
Understanding Familial Cholesterol Conditions
Familial cholesterol conditions are inherited disorders that greatly affect health. They usually show up as high cholesterol levels in the blood, leading to heart problems if not treated. Knowing about these disorders can help catch them early and manage them well, improving health.
Different Types of Inherited Cholesterol Disorders
Familial hypercholesterolemia (FH) is a major inherited cholesterol issue affecting around 1.3 million in the U.S., including kids. It’s estimated that one in 200 adults has the genetic mutation for FH. FH comes in two main types:
- Heterozygous FH (HeFH): This more usual form can push LDL cholesterol over 190 mg/dL in serious cases.
- Homozygous FH (HoFH): This rarer version comes from both parents, with LDL cholesterol levels going above 400 mg/dL.
Other inherited cholesterol disorders like PCSK9-related conditions and lipoprotein(a) disorders can also spike cholesterol levels. Some ethnic groups, such as those from French Canadian, Ashkenazi Jewish, Lebanese, or Afrikaner backgrounds, have a higher chance of having these conditions.
Diagnosing and Treating Inherited Conditions
Getting these cholesterol disorders correctly diagnosed is key. Cascade screening helps find individuals at risk, especially if FH runs in their family. Sadly, over 90% with familial hypercholesterolemia don’t know they have it, which underlines the importance of better awareness.
The treatment approach depends on how severe the disorder is. Medicines like statins are often used to cut LDL cholesterol by at least 50%. For extreme cases, like with HoFH, LDL apheresis might be needed to remove extra cholesterol. PCSK9 inhibitor injections are another treatment option.
It’s advised to test children at risk for FH starting at age two. Catching it early lets doctors manage it better, leading to improved health outcomes and lower risk of heart attacks or strokes from these inherited cholesterol problems.
| Inherited Disorder | Common Characteristics | Treatment Options |
|---|---|---|
| Familial Hypercholesterolemia (FH) | High LDL levels, varies by type | Statins, PCSK9 inhibitors, LDL apheresis |
| PCSK9-related disorders | High levels of LDL cholesterol | Medications targeting PCSK9 |
| Lipoprotein(a) disorders | Elevated lipoprotein(a) levels | Statins and lifestyle changes |
Can High Cholesterol Be Inherited?
High cholesterol can be passed down in families. This is called inherited cholesterol risk. One common condition is familial hypercholesterolemia (FH). It’s often missed, with most people not knowing they have it. Understanding FH is key in families with heart disease history. It helps in catching the condition early.
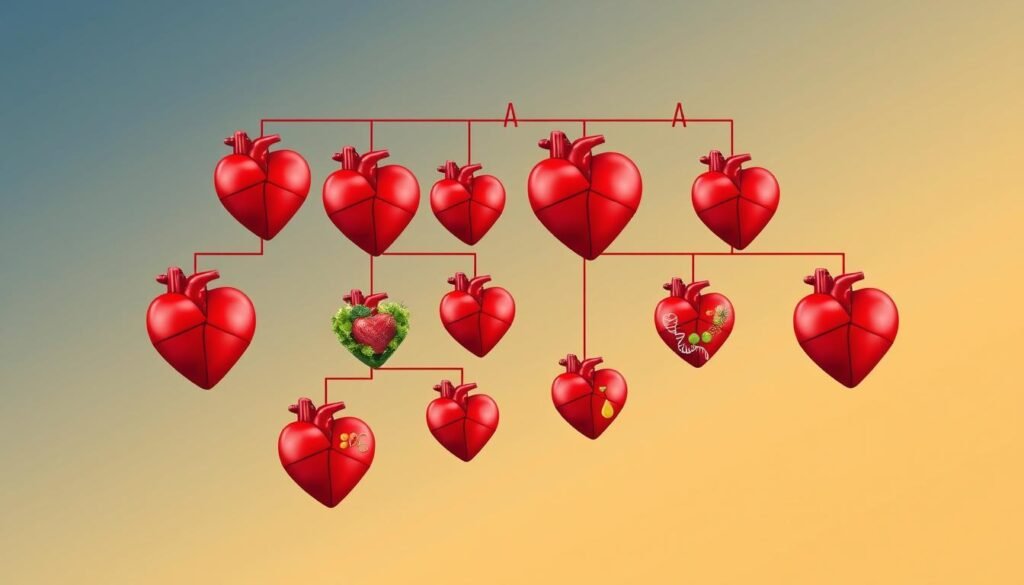
Genetic Transmission of Familial Hypercholesterolemia
FH can move down through generations. Children have a 50% chance of getting it from one parent. The risk doubles if both parents have FH. The rare homozygous FH leads to very high LDL cholesterol, sometimes over 400 mg/dL. Heterozygous FH, from one parent, can push levels above 190 mg/dL.
Testing Family Members: When to Start
Finding which family members might have FH is key. Cascade screening helps identify them. Testing is a must if heart disease shows up early in the family. Early detection and action are crucial. Lifestyle changes and medications are helpful. They can lower bad LDL cholesterol. For tips on managing cholesterol, check out this helpful guide.
Impact of Lifestyle on Genetic High Cholesterol
Genetic factors play a big role in your cholesterol levels. But, lifestyle choices are also key. Even if you have a genetic condition like familial hypercholesterolemia, you can still improve your health. By eating a balanced diet and exercising regularly, you can better manage your cholesterol.
How Diet Can Influence Cholesterol Levels
A balanced diet is crucial for keeping cholesterol in check. Eating lots of saturated and trans fats can raise your bad cholesterol (LDL), upping heart disease risk. On the flip side, eating more fruits, veggies, whole grains, and healthy fats (think avocados and olive oil) can aid in maintaining a healthy cholesterol level. It’s important to eat saturated fats sparingly, no more than 10% of your daily calories. Also, omega-3 rich foods like salmon can help lower your total cholesterol and boost heart health.
Exercise: A Key Factor in Cholesterol Management
Staying active is equally important in managing cholesterol. Activities like jogging, swimming, or cycling boost heart health and reduce bad cholesterol. Regular exercise can lower LDL cholesterol by up to 10%. Plus, it reduces stress, helps keep your weight in check, and enhances your overall well-being.
| Factor | Impact on Cholesterol |
|---|---|
| High saturated fat intake | Increases LDL cholesterol levels |
| Regular aerobic exercise | Can lower LDL cholesterol and raise HDL cholesterol |
| Smoking | Reduces HDL cholesterol, raises LDL cholesterol |
| Excessive alcohol consumption | Elevates total cholesterol levels |
| Poor sleep quality | Linked to reduced cardiovascular health |
Making lifestyle changes is doubly important for those with a genetic risk of high cholesterol. Every healthy decision improves your cholesterol levels. This supports your efforts to tackle the condition with diet and exercise.
Preventing Heart Disease Related to High Cholesterol
Preventing heart disease is crucial, especially for those at risk, like people with FH. Keeping an eye on cholesterol levels and being proactive about health is key. These steps are vital for keeping your heart healthy.
Heart Health Strategies for Those with FH
If you have FH, you’re more likely to get heart disease because of high LDL (bad cholesterol) levels. It’s very important to use effective strategies for your health. Doctors often recommend:
- Regular screenings to monitor cholesterol levels.
- Following a heart-healthy diet, low in saturated fats.
- Engaging in at least 150 minutes of moderate-intensity aerobic exercise each week.
- Staying informed about familial health history and its role in heart disease.
- Consulting healthcare professionals for personalized treatment plans, which may include medication.
The Importance of Early Detection and Treatment
Catching high cholesterol early can really help in stopping heart disease. A lipid panel blood test is a good way to find out your cholesterol levels early. Sadly, less than 10% of people with FH know they have it. Without treatment, their LDL levels could shoot up, which is dangerous.
Getting ahead of the problem can lower the risk of serious issues like heart attacks or strokes. Talking to doctors about heart health symptoms is important. Spotting things early leads to better health results.
| Cholesterol Type | Role in Heart Health |
|---|---|
| LDL (Low-Density Lipoprotein) | Considered bad cholesterol; accumulates in arteries |
| HDL (High-Density Lipoprotein) | Regarded as good cholesterol; helps in removing LDL from arteries |
Focus on prevention and early treatment is key. It can help you keep a strong and healthy heart for life.
Future Research on Cholesterol Genetics
Cholesterol genetics is an exciting field that can lead to new treatments. Scientists are learning how genes control cholesterol levels. This could change how we treat genetic high cholesterol.
New Developments in Genetic Treatments
Studies show that our genes strongly influence HDL (High-Density Lipoprotein) cholesterol. This is important because low HDL-C levels often occur in patients with coronary artery disease (CAD). Understanding genes like APOA1, ABCA1, and CETP may lead to new therapies to increase HDL levels. This could lower CAD risk significantly.
The Potential for Gene Therapy
Gene therapy targets genetic issues causing abnormal cholesterol levels. For instance, lack of ApoAI can cause very low HDL and high CAD risk. On the other hand, CETP deficiency can significantly raise HDL levels. Correcting these genetic conditions may offer major heart health benefits. Studying different ancestries helps in creating personalized cholesterol treatments for everyone.
| Gene | Condition | Typical HDL Levels | Risk Factor |
|---|---|---|---|
| APOA1 | ApoAI deficiency | Extremely low ( | Increases risk of CAD |
| CETP | CETP deficiency | High (>100 mg/dl) | Possible increased apoAI |
| LCAT | LCAT deficiency | Low | Varied clinical findings, CAD |
| ABCA1 | Genetic mutations | Variable | Impact on HDL metabolism |
Conclusion
It’s crucial to grasp the link between genetics and high cholesterol for better handling and stopping heart issues. This is especially true for conditions like familial hypercholesterolemia (FH). Studies have found that 17.1% of people with high cholesterol have genetic reasons for it. This shows how big a role genetics plays.
About 8.4% of people studied were found to have the FH phenotype. This highlights how vital it is to be aware and catch this condition early. Knowing about familial hypercholesterolemia helps us understand the risks. If ignored, these risks can lead to severe health problems.
Nearly 26% of those who meet the FH clinical guidelines have genetic factors. This points to ways we can directly tackle the problem. Using medicines like statins, along with changing our lifestyle, can greatly help. It can keep our hearts healthy for years to come.
Making early screening and knowing our family’s health history a priority can lower the risk of heart disease linked to high cholesterol genetics. By increasing awareness and access to genetic testing, the medical community can empower us. We can take on familial hypercholesterolemia. This leads to a healthier future for all of us.