Did you know nearly 25 million adults in the US have very high cholesterol? This fact shows a lot of people have hyperlipidemia. This means their blood has too much fat. It’s bad for the heart. Learning to code high cholesterol with the ICD-10 system is key for doctors. It helps with patient care and billing. This guide will explain the basics of high cholesterol, its risks, and how to code it.
Key Takeaways
- Approximately 25 million adults in the U.S. are affected by high cholesterol levels.
- Children and adolescents also face risks, with about 7% having high total cholesterol.
- Untreated hyperlipidemia significantly increases the likelihood of coronary artery disease.
- Different ICD-10 codes classify various types of hyperlipidemia and their severities.
- Accurate coding is vital for both patient care and reimbursement in medical billing.
Understanding Hyperlipidemia
Hyperlipidemia is when there’s too much lipid, like cholesterol, in the blood. It’s key to know about it to manage heart health and for correct healthcare coding.
Definition of Hyperlipidemia
Hyperlipidemia means higher than normal lipid levels in your blood. It can cause severe health problems. There are different types, such as high cholesterol, mixed types, and high triglycerides. Each kind affects your risk for heart disease differently.
Causes of Elevated Lipid Levels
Many things can make lipid levels go up. It’s important to know these to prevent and handle them. Some major causes are:
- Unhealthy dietary habits: Eating too much saturated fats, trans fats, and cholesterol.
- Sedentary lifestyle: Not being active can slow down fat processing in your body.
- Genetic predisposition: Some people have genes making them prone to high lipids.
Cardiovascular Implications of Hyperlipidemia
Those with untreated hyperlipidemia are at greater risk for heart issues. They’re twice as likely to get coronary artery disease compared to those with healthy lipid levels. High lipids can lead to atherosclerosis, risking heart attacks or strokes. Knowing these risks helps in evaluating patients and making coding choices.
Symptoms of High Cholesterol
It’s vital to know the signs of high cholesterol for your health. Often, high cholesterol doesn’t show clear symptoms until it leads to major health problems. This is why getting checked regularly is key for catching and managing it early.
The Silent Nature of Hyperlipidemia
Hyperlipidemia, or high cholesterol, is called a silent condition because you might not see any signs. Many don’t know they have it until they face serious issues like heart diseases. Being aware is crucial, as heart issues can show up as chest pain or difficulty breathing later on.
Importance of Regular Screening
Getting your cholesterol checked regularly is very important. Experts say people, especially if they have a family history of heart problems or are overweight, should get screened every five years. Early detection through screenings can help you take steps to avoid bigger health problems.

High Cholesterol ICD 10: Accurate Coding Essentials
Getting hyperlipidemia documented right is key in healthcare. It affects both patient care and insurance. The ICD-10 coding system helps by classifying different types of hyperlipidemia clearly. This ensures better record-keeping and communication among healthcare teams. Knowing the right codes helps in better coding and patient management.
ICD-10 Code Overview for Hyperlipidemia
ICD-10 codes for hyperlipidemia include specific codes for accurate billing and record-keeping. Here are the main codes for hyperlipidemia:
| ICD-10 Code | Description |
|---|---|
| E78.00 | Pure hypercholesterolemia (high LDL cholesterol) |
| E78.01 | Familial hypercholesterolemia (genetically inherited high cholesterol) |
| E78.1 | Pure hyperglyceridemia (high triglycerides) |
| E78.2 | Mixed hyperlipidemia (elevated LDL and triglycerides) |
| E78.4 | Other hyperlipidemia |
| E78.5 | Hyperlipidemia, unspecified |
Importance of Specificity in Coding
Specific codes in ICD-10 are crucial for precise hyperlipidemia documentation. They allow for better treatment and accurate insurance payments. Using a general code like E78.5 can lead to poor treatment choices. It may even cause issues in patient care. Exact codes help doctors make the best decisions for their patients’ health.
Lifestyle changes and new diagnostic tech also play a big role in treating hyperlipidemia. These advances can really help in managing cholesterol. For deeper understanding of cholesterol and related issues, check out this resource.
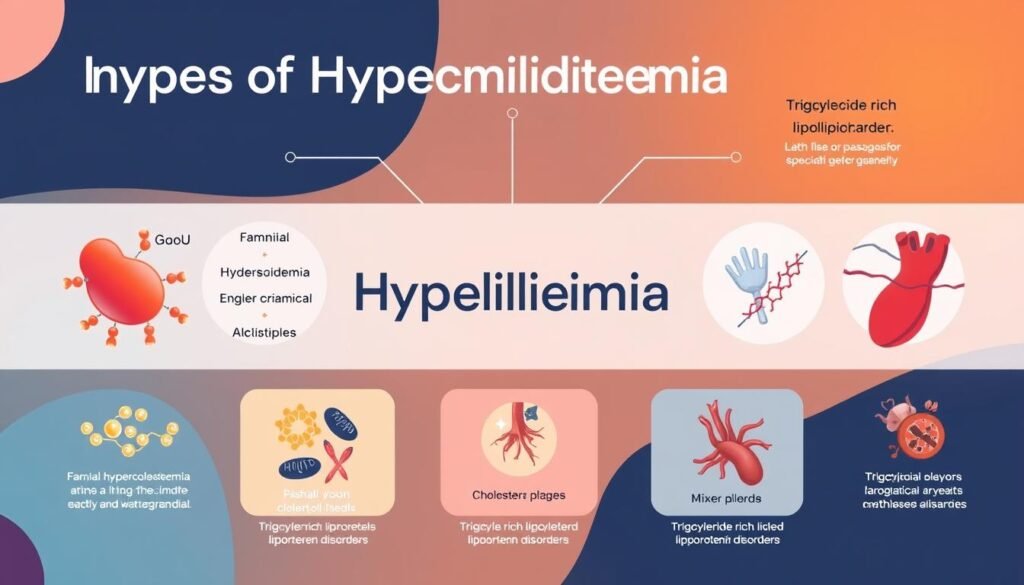
Types of Hyperlipidemia and Relevant ICD 10 Codes
Hyperlipidemia includes different types, each with a specific ICD-10 code. It’s vital to know these codes for effective treatment and billing. Around 94 million adults have high cholesterol. This makes precise coding crucial. Here are the hyperlipidemia types and their ICD-10 codes.
Pure Hypercholesterolemia and its Code (E78.00)
Pure hypercholesterolemia is noted by ICD-10 code E78.00. It’s when cholesterol in the blood is too high. Managing this is key to avoiding heart issues. Using this code, doctors can create focused treatments.
Familial Hypercholesterolemia (E78.01)
Familial hypercholesterolemia gets ICD-10 code E78.01. It’s a genetic issue causing very high cholesterol. Spotting it early and coding it right is key for good care.
Mixed Hyperlipidemia (E78.2)
Mixed hyperlipidemia is marked by ICD-10 code E78.2. It means both cholesterol and triglycerides are too high. Understanding this helps doctors plan better treatments for patients.
Doctors can find coding help for hyperlipidemia at resources like this guide. The right ICD-10 codes improve patient care and outcomes.
Distinguishing Between Hyperlipidemia and Dyslipidemia
To effectively care for patients and code medical conditions, it’s vital to know the difference between hyperlipidemia and dyslipidemia. Hyperlipidemia means there’s too much cholesterol and triglycerides in the blood. Dyslipidemia covers all abnormal lipid levels, including too low or too high. This distinction affects how doctors document and treat these conditions.
Definitions and Differences
Individuals with hyperlipidemia have high levels of LDL cholesterol and triglycerides. Dyslipidemia includes a wider variety of lipid problems. It’s important to understand these terms to ensure correct coding. E78.5 is often used to document dyslipidemia. Knowing the difference helps select the right treatments and monitoring plans.
Impact on Coding Practices
Correctly telling apart hyperlipidemia and dyslipidemia is crucial for medical coding. Codes need to accurately show a patient’s lipid levels for the best care. Wrong codes can lead to the wrong treatment and bad outcomes for patients. Coders need to keep up with the latest information to handle these complex conditions well.
| Condition | Description | ICD-10 Code |
|---|---|---|
| Hyperlipidemia | Elevated lipid levels in the blood, primarily cholesterol and triglycerides. | E78.00, E78.01, E78.2 |
| Dyslipidemia | Any abnormal level of lipids in the blood, including both high and low levels. | E78.5 |
Lipid Metabolism and its Role in Cholesterol Management
Lipid metabolism is key in controlling cholesterol. It affects how the body handles fats and cholesterol. Knowing lipid profiles helps doctors check cholesterol and triglyceride levels. This guides plans for those at risk of high blood fats. Lipid profiles give crucial details for decisions on heart health.
Understanding Lipid Profiles
Lipid profiles show levels like total cholesterol, LDL-C, HDL-C, and triglycerides. These levels help figure out heart disease risk:
| Cholesterol Type | Desirable Level | Borderline Level | High-risk Level |
|---|---|---|---|
| Total Cholesterol | Less than 200 mg/dL | 200-239 mg/dL | 240 mg/dL and above |
| LDL-C | Less than 100 mg/dL | 100-129 mg/dL | 130 mg/dL and above |
| HDL-C | 60 mg/dL and above | 40-59 mg/dL | Less than 40 mg/dL |
| Triglycerides | Less than 150 mg/dL | 150-199 mg/dL | 200 mg/dL and above |
The Role of Lifestyle Factors
Lifestyle greatly impacts lipid metabolism and cholesterol control. A good diet and exercise can improve lipid profiles. This helps lower the risk of heart disease. Changes to make include:
- Eating well with lots of fruits, veggies, whole grains, and lean meats
- Being active for 150 minutes a week
- Cutting down on trans and saturated fats
- Keeping a healthy body weight
- Stopping smoking and limiting alcohol
Knowing how lifestyle and lipid metabolism link helps us manage cholesterol better.
Guidelines for Accurate ICD 10 Coding
Getting ICD-10 coding right is key for showing patient issues and getting correct payments. The ICD 10 coding guidelines emphasize checking medical documentation closely. This ensures diagnoses are as detailed as possible. This step is crucial, especially for conditions like hyperlipidemia. It helps health workers and coders work together better. This makes sure coding is accurate, supporting both great patient care and fair payment.
Reviewing Medical Documentation
Good medical documentation is the base for effective coding. Every piece of patient info must be noted accurately. This includes their history and any other health issues they have. The American Hospital Association (AHA) and Centers for Medicare and Medicaid Services (CMS) highlight how important this is. To get more info on this, check the ICD-10-CM Official Guidelines.
Choosing the Right Code for Treatment
It’s crucial to pick the right ICD-10 code for each patient. This ensures they get the right care. Doctors need to know codes like E78.00 for pure hypercholesterolemia and E78.5 for hyperlipidemia that’s not specified. Knowing this helps with correct reporting. When healthcare workers talk well and follow the ICD 10 coding guidelines, patients get the care they need. Plus, it helps with getting correct payment.
Implications of Misdiagnosing High Cholesterol
When doctors misdiagnose high cholesterol, it creates big problems. It’s important to get the diagnosis right to ensure patients get the correct treatment. This reduces their risk of heart disease, heart attacks, and strokes. Not catching high cholesterol levels can lead to bad health outcomes, showing how crucial accurate diagnosis is.
Consequences for Patient Care and Safety
Getting high cholesterol wrong can be dangerous for patients. Studies link LDL-C levels of 100 mg/dL or higher with a greater risk of heart disease. Those misdiagnosed might miss out on essential treatments. This can increase the chance of serious heart problems. For example, research over six years showed nearly 52,000 heart-related issues due to wrong diagnoses and treatments.
Reimbursement and Insurance Considerations
Misdiagnosis affects not just health but also finances. If doctors don’t accurately record high cholesterol, insurers might not cover treatment costs. This misstep can put a financial burden on hospitals and clinics. They struggle to get paid by insurance for treatments given. Accurate coding is key in healthcare to ensure treatments are paid for and patients get what they need.
| Diagnosis | Potential Risks | Insurance Impact |
|---|---|---|
| Correct Diagnosis of High Cholesterol | Reduced CVD risk, appropriate management | Improved reimbursement reliability |
| Misdiagnosis of High Cholesterol | Increased cardiovascular events, higher mortality | Risk of denied claims, financial losses |
Conclusion
For healthcare experts, understanding how to manage high cholesterol is key. This is because of the big impact hyperlipidemia can have. The study of different diagnostic tools like the Dutch Lipid Network Criteria (DLNC) shows the need for careful medical records.
Different ways of identifying the condition help doctors treat patients better. This can lead to improved health for those affected.
Research with over 269,391 people over 40 years old shows the dangers of high cholesterol. Those with higher levels faced a greater risk of dying. This fact highlights how vital precise ICD-10 coding is. It helps doctors treat patients more effectively. To learn more about the challenges in identifying familial hypercholesterolemia, click here.
As the concern over high cholesterol grows, it’s important for healthcare workers to stay updated. By understanding ICD-10 codes for lipid disorders, they can offer better care. This approach improves patient health and the quality of healthcare provided.